A little over seventeen years ago around this time I started coming down with flu-like symptoms. My father already had similar symptoms, and my mother developed them shortly after. After a week our symptoms only got worse. So, we went to our doctor. He suspected a bacterial infection and prescribed an antibiotic: tetracyclin. This helped: within four days most of the infection cleared, and within two weeks all lingering symptoms disappeared.
The Ancient
Antibiotics may conjure up an image of people wearing white coats in a modern laboratory. However, traces of that same antibiotic we used, tetracyclin, were found in ancient mummies. How could this be?
We often think of medication as something made in a lab. However, antibiotics, stuff that either kills or slows the growth of bacteria, are all around us. Humans have been consuming antibiotics for a long time, though without knowing the actual mechanism behind their curing effects.
Antibiotics found in the soil are a natural byproduct of warfare at a tiny scale. As bacteria compete with other bacteria to survive, producing something that kills the competition is a highly effective survival strategy. The result of this small-scale chemical warfare can both help us and harm us.
The Great War
Anyone who went to Sam Mendes’s 1917, a film about the first World War, got at least an inkling of what it was like back then. However, while brilliantly shot, some of the trenches looked a bit too clean.

In reality the hygienic conditions in the trenches of World War I were abysmal. The spread of disease made worse by decaying corpses, poor sanitation and prolific bugs such as lice and flies. Combined with the soldiers’ own weakened immune systems and the transport of livestock near the front-lines, the environment formed the perfect breeding ground for existing diseases to flourish and new ones to emerge. While the macroscopic trench warfare was characterized by stand-offs, the microscopic germ warfare was continuous.
The Spanish Flu
Near the end of the war a new kind of flu emerged in northern France, one with an unusually high mortality rate. To maintain the morale of the troops, the news of this novel flu was mostly kept under wraps. However, as the infection spread to Spain, not subject to this censorship, reports of its devastating death toll started to spread more widely. This owed the disease its popular name: The Spanish flu.
The Spanish flu quickly spread to Ireland through returning soldiers. Saved from the brutal war, some of them would become the carriers of death for the home front. The disease spread throughout the United States and the rest of the world and killed about two people for every ten infected. In total it would go on to claim at least fifty million lives worldwide.

No antibiotic existed yet, but none would have helped directly against this flu either, since antibiotics combat bacterial infections not viral ones. Nevertheless, antibiotics could have saved the lives of many soldiers during World War I. Especially those with infected wounds and diseases like typhoid. However, it would take another decade for the first antibiotic to be found.
Fungi Fighters
In 1928 Alexander Fleming discovered this first antibiotic more or less by accident: penicillin. During the second World War, the availability of penicillin saved many lives. However, while useful for resolving and preventing bacterial infections, it was ineffective against fungal diseases which many came down with. Hence, focus shifted from bacteria to fungi. The race was on to find something that would kill those fungi.
Elizabeth Hazen, a bacteriologist, dedicated years of her life to the search for an antifungal producing microbe. She scouted soil samples and mailed them to Rachel Brown, a chemist, for purification. The pair searched for several years and during that time discovered many molecules that proved lethal to both fungi and animals. One day Elizabeth found a promising micro organism in a soil sample of a friend’s dairy farm.

Fortunately, the organism produced a molecule that killed only fungi and not animals. Hazen and Brown marketed it as Nystatin, the world’s first antifungal drug. It saved countless lives since its introduction. The patent on the drug made them millionaires. Money which they donated to a nonprofit that went on to conduct similar research.
The Modern World
In recent years we have seen outbreaks of several high-profile influenza viruses with a higher than usual mortality rate. Think of SARS (2003), MERS (2012) and recently COVID-19 (2019). Like the Spanish flu, outbreaks like these have the potential to wreak havoc. However, while public awareness concerning the emergence of novel viruses is high, the risks of infections with mutated resistant bacteria, and fungi, are understated. After all, we already have antibiotics and antifungals to combat and defeat those, right?

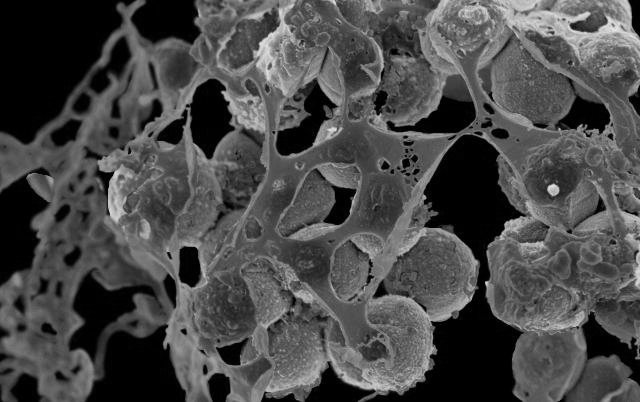
Unfortunately, that has not been the case for many years. The best known example is MRSA: methicilin-resistant Staphylococcus aureus. Dairy cows serve as a reservoir for this family of mutated strains of the common and normally harmless Staphylococcus aureus bacterium.
The overuse and misuse of penicillin in the fifties contributed to the evolution of resistant strains of Staphylococcus aureus. Methicillin was then used instead to fight it, but over time resistant strains emerged: MRSA. Nowadays, the treatment for it is Vancomycin, but there are already mutations for which that treatment no longer seems to be as effective.
The circumstances that gave rise to widespread bacterial infections during World War I, still exist. There are plenty of overcrowded places with poor sanitation, proximity to animals treated with antibiotics which harbor resistant microbes, and lackluster medical facilities and dismal containment procedures. The ideal breeding ground for the next fatally resistant mutation. This risk is thus not restricted to viruses, but extends to bacteria and fungi alike.
These resistant microbes spread and thrive in places where people gather or pass through like hospitals. Their presence there can turn routine operations into risky procedures.
In conclusion
While the discovery of antibiotics is fairly recent, they have existed for many years in the soil. This continues to be a source for development of new drugs, so too for antifungals.
Poor hygienic condition provide a breeding ground for new bacteria, fungi, viruses and other pathogens to mutate into something more deadly. Finding an effective treatment can take many years, if one can be found at all.
While viral mutations are risky, so are mutations of bacteria and fungi. The treatments that we currently have for them can lull us into a false sense of security. This is why we should take care to protect our most potent antibiotics and antifungals. We should do this by using them judiciously, limiting their applications in agriculture, and incentivizing work on continuously finding new ones.
I conclude with the jarring realization that if there had not been antibiotics available, effective against the bacterial infection my family contracted, we might not have experienced the past seventeen years at all.
References
- McCarthy, M. (2019). Superbugs: The Race to Stop an Epidemic.
- Jackson, P. (2019). They shall not grow old.
- Jacobs, A. (2019). U.N. Issues Urgent Warning on the growing Peril of Drug-Resistant Infections.